- 1Department of Medical Education, University of Miami Miller School of Medicine, Miami, FL, United States
- 2Department of Obstetrics, Gynecology, and Reproductive Sciences, Jackson Memorial Hospital, Miami, FL, United States
- 3Division of Gynecologic Oncology, Sylvester Comprehensive Cancer Center/University of Miami Miller School of Medicine, Miami, FL, United States
Introduction: Vaccination against HPV is safe and effective in cancer prevention, yet vaccination uptake remains low. Strong recommendation of HPV vaccination by healthcare providers increases immunization rates, but gaps in knowledge persist surrounding HPV and HPV vaccination amongst health professional students (HPS). It is critical to educate HPS in all professions to maximize vaccination opportunities and increase vaccine uptake. The objective of this study is to evaluate evidence on HPV knowledge, vaccine uptake, and educational interventions in HPS to identify specific deficits to improve education.
Methods: A systematic literature search for articles on HPV vaccine uptake, knowledge, and educational interventions in HPS was performed in PubMed, Embase, Web of Science, CINAHL, and Scopus from January 1, 2006 – July 21, 2021. Included studies assessed HPS for HPV vaccine uptake, knowledge, counseling comfort, or educational interventions to increase HPV vaccine knowledge. Studies were screened for inclusion by 2 independent reviewers and evaluated for risk of bias. PRISMA guidelines for reporting were followed.
Results: Twenty-one unique articles met inclusion criteria and were included in the analysis. Of the studies included, 20 included knowledge, 11 included vaccine uptake, 8 included interventions, and 12 included counseling comfort. The students in the studies included medical (n=14), dental (n=7), dental hygiene (n=6), nursing (n=3), physician assistant (n=2), public health (n=1), and pharmacy (n=1). Across studies, HPV vaccine series initiation ranged from 34.6-70.3%, with 28.3-58.3% up to date on vaccination. Most students knew that HPV causes cervical cancer (99%), but fewer knew that HPV causes head and neck cancer (40-47%) and oropharyngeal cancer (45%). Educational interventions included team-based approaches and lectures, and improved outcomes including vaccine knowledge, vaccination schedule, and cancer knowledge. Medical students with lower knowledge of HPV were more hesitant to recommend vaccination at baseline but were more likely to recommend vaccination after an education session.
Discussion: Across HPS, inadequacies persist in HPV vaccine uptake, knowledge, and counseling comfort. It is critical to target vaccine uptake in this population and improve existing educational efforts to reduce preventable cancers. Institutions must prioritize HPV vaccine education to impact HPV related death.
Introduction
In the US approximately 36,500 preventable cancers attributed to HPV are diagnosed yearly (1). Worldwide, 690,000 cases of cancers attributed to HPV are diagnosed each year (2). The most common HPV related cancer in women is cervical cancer, and in men is oropharyngeal cancer (3). While the incidence of cervical cancer has decreased over the past 15 years, there has been a significant increase in incidence rates of oropharyngeal, anal/rectal, and vulvar cancers (4).
HPV vaccination, first approved by the FDA in 2006 (5), is a safe and effective method to prevent HPV related cancers, and has substantially reduced the risk of invasive cervical cancer (6). The advisory council on immunization practices recommends routine HPV vaccination between ages 9-12, and catch up vaccination up to age 26 (7). For adults age 27-45, shared decision making is recommended to determine if a patient would benefit due to an elevated risk of HPV (7).
Unfortunately, the nation fell well below the Healthy People 2020 goal to achieve a HPV vaccination rate of 80%, with only 53% of females and 46% of males between 13-17 years up to date on HPV vaccination (8, 9). HPV vaccination is paramount to cancer prevention strategies. However, despite evidence of HPV vaccine safety, the rate of those citing safety concerns as the reason to not initiate the HPV vaccine series has increased 79.8% between 2015 and 2018 even though the rate of adverse events reported decreased to 29.4% in the same period (10). While evidence shows that the HPV vaccine is safe, patients continue to decline vaccines for reasons not backed in evidence including a belief that HPV vaccines are only for girls, should not be initiated prior to sexual debut, and is only approved up to age 15 (11). Myths and misinformation surrounding the HPV vaccine have been prevalent and active debunking of these myths by healthcare providers is critical (12–14).
To increase HPV vaccination rates, education surrounding HPV vaccine must be improved for healthcare providers in all fields. HPV vaccines are the only cancer prevention vaccine currently available, and it is a responsibility of all healthcare providers to recommend the vaccine and utilize all opportunities to vaccinate patients. With an intensification in vaccine hesitancy, it is important to confidently ensure parents that HPV vaccination is safe (10). Strong recommendation for HPV vaccine by a healthcare provider has been positively associated with vaccine uptake (15). HPV vaccination can be obtained in a variety of settings beyond the doctor’s office including schools (nurses) (16), pharmacies (17–19), and dental offices (20, 21). Efforts to increase HPV vaccine uptake must be recognized as an interprofessional mission by empowering HPS in a variety of professions to become vaccine champions. However, low fund of knowledge contributes to lack of confidence in recommending HPV vaccination across professions (19, 22–26). Additionally, previous work has shown that HPS who are vaccinated against HPV are significantly more likely to recommend HPV vaccines to their patients (27).
HPS must receive comprehensive education on HPV and HPV vaccines while in the formal learning environment. While several single-institution studies have assessed HPV knowledge and performed associated educational interventions, the efficacy and merits of these interventions have not been weighed against one another. Previous systematic reviews have synthesized educational interventions surrounding HPV vaccines in practicing healthcare providers, but not in HPS (24). The objective of our study was to evaluate the uptake of HPV vaccines, current HPV vaccine education initiatives, and HPV vaccine knowledge deficits in HPS.
Methods
Search strategy
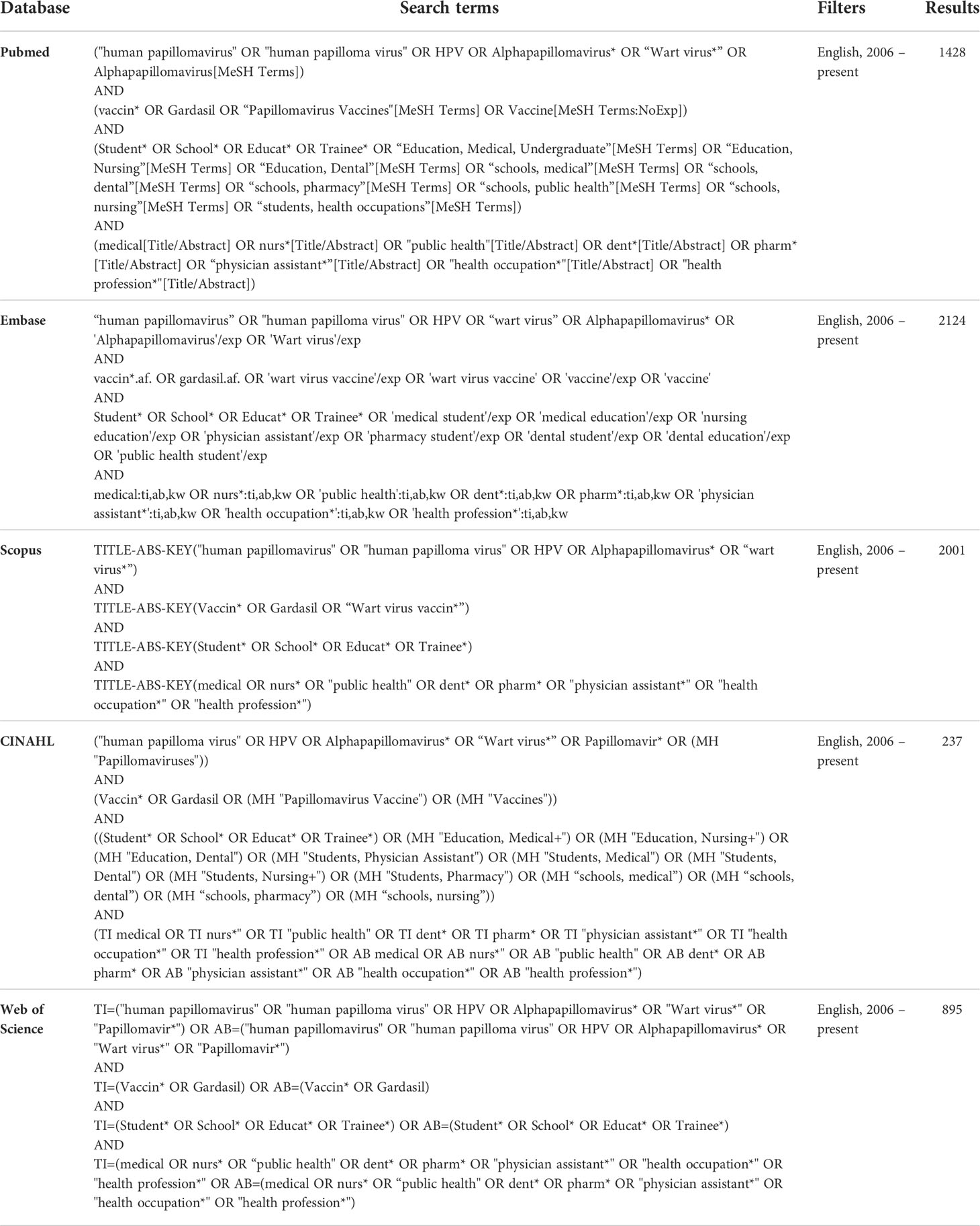
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline was used as a framework to guide the design and reporting of our study (28). We performed a systematic literature search from January 1, 2006, to July 21, 2021, to identify studies using the following databases: PubMed, Embase, Scopus, Web of Science, CINAHL. Articles prior to 2006 were not included because the HPV vaccine was not available. A previous systematic review on HPV knowledge among providers was reviewed for search term ideas (24). The complete search strategy is reported in Table 1.
Following the completion of searches, all articles identified were exported into EndNote and duplicates were removed. Articles were then imported into Covidence. First, titles and abstracts were reviewed independently by two reviewers (ML, LF, MH). Next, full text articles were obtained and reviewed by two reviewers. Following this, articles were screened for risk of bias by two reviewers to assess methodologic quality. Disagreements between reviewers were resolved by the third reviewer. Finally, data extraction was performed in covidence by two reviewers. A third reviewer compared results of data extraction by both reviewers to compile the final data which was exported for analysis.
For this review, HPS were defined as students in health professions that prescribe or promote HPV vaccination in their practice including medicine, nursing, pharmacy, public health, dentistry, and physician assistant. In studies that included practicing providers with students, >50% of the participants had to be students for inclusion. Inclusion criteria were as follows: 1) Original articles published in a peer-reviewed English language journals including quantitative, experimental, qualitative, quasi-experimental and observational studies. 2) Students attending school in the US due to the heterogeneity of health professional education worldwide. 3) Articles published in 2006 or later. 4) Studies with an objective to evaluate HPV vaccine uptake in HPS, knowledge of HPV vaccines in HPS, an educational intervention to improve knowledge of HPV vaccines in HPS, and/or HPS comfort counseling about HPV vaccination. Comfort counseling was defined as self-reported increase in confidence in counseling patients and/or their parents about HPV vaccination. The exclusion criteria were as follows: 1) Articles without full text, commentaries, editorials, perspective pieces, conference abstracts. 2) Studies of practicing healthcare providers including residents, fellows, nurses, dentists, pharmacists, physician assistants. Residents and fellows were excluded to focus on students in undergraduate medical education. 3) Studies of undergraduate students who were not in differentiated professional degree programs such as nursing.
Data and analysis
The risk of bias was assessed with the Joanna Briggs Institute Tool for Cross Sectional Studies (29). The results of the risk of bias screening appear in Table 2. This tool encompasses inclusion criteria, whether the study subjects and setting were described in detail, exposure measurement in a valid and reliable way, confounding factors, strategies to deal with confounding factors, outcome measurement in a valid and reliable way, and appropriate use of statistics. Full text papers to be included were assessed for risk of bias by two independent reviewers by appraising the papers based on this criterion. Disagreements between reviewers were resolved by the third reviewer. All articles included in the study were reviewed based on this process.
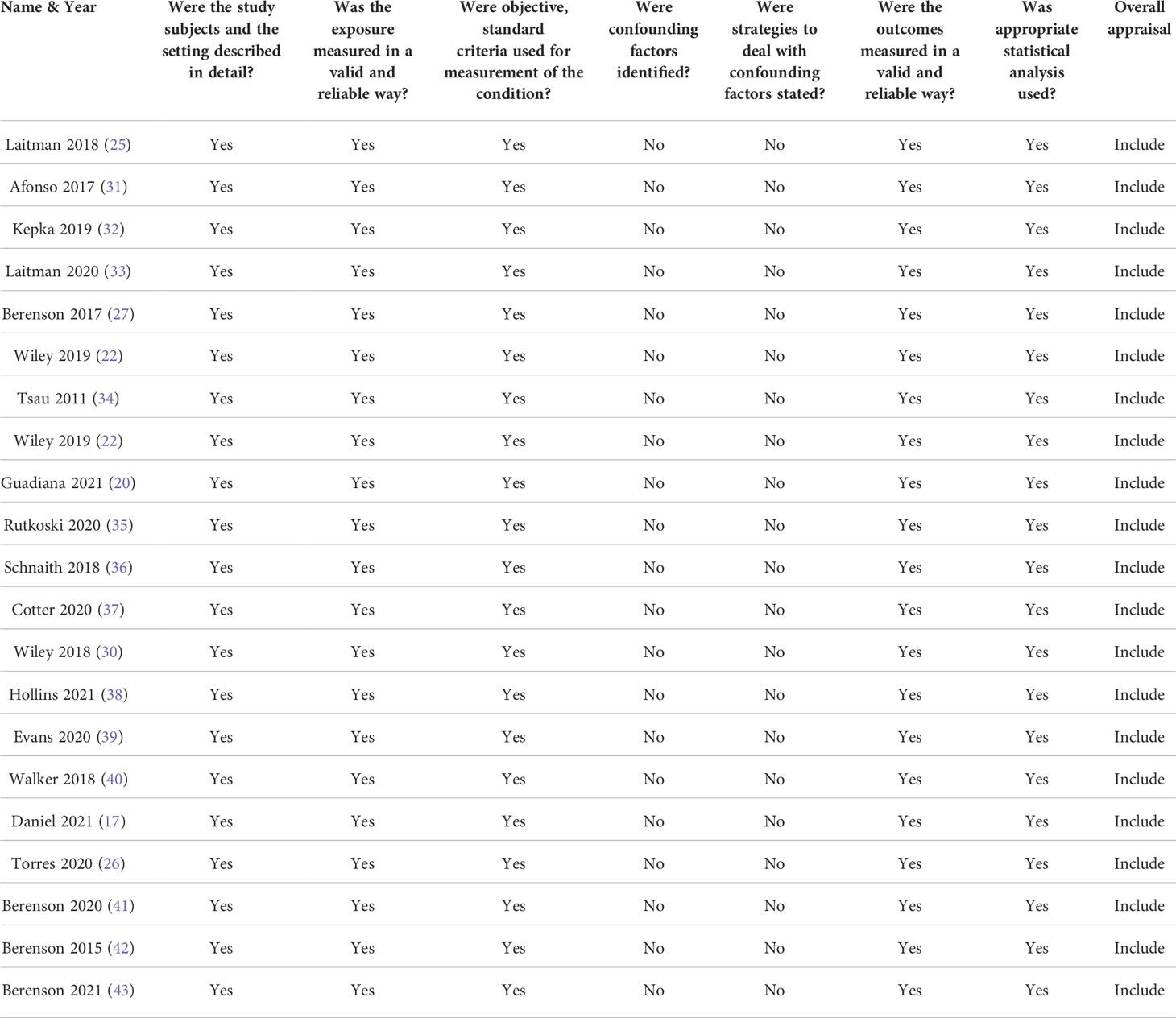
Table 2 Risk of Bias Evaluation (30).
Studies selected for inclusion had data extracted by two independent reviewers. The Template for Intervention Description and Replication (TIDiEr) checklist was used to develop the data collection for HPV knowledge interventions (44).
Results
Literature search
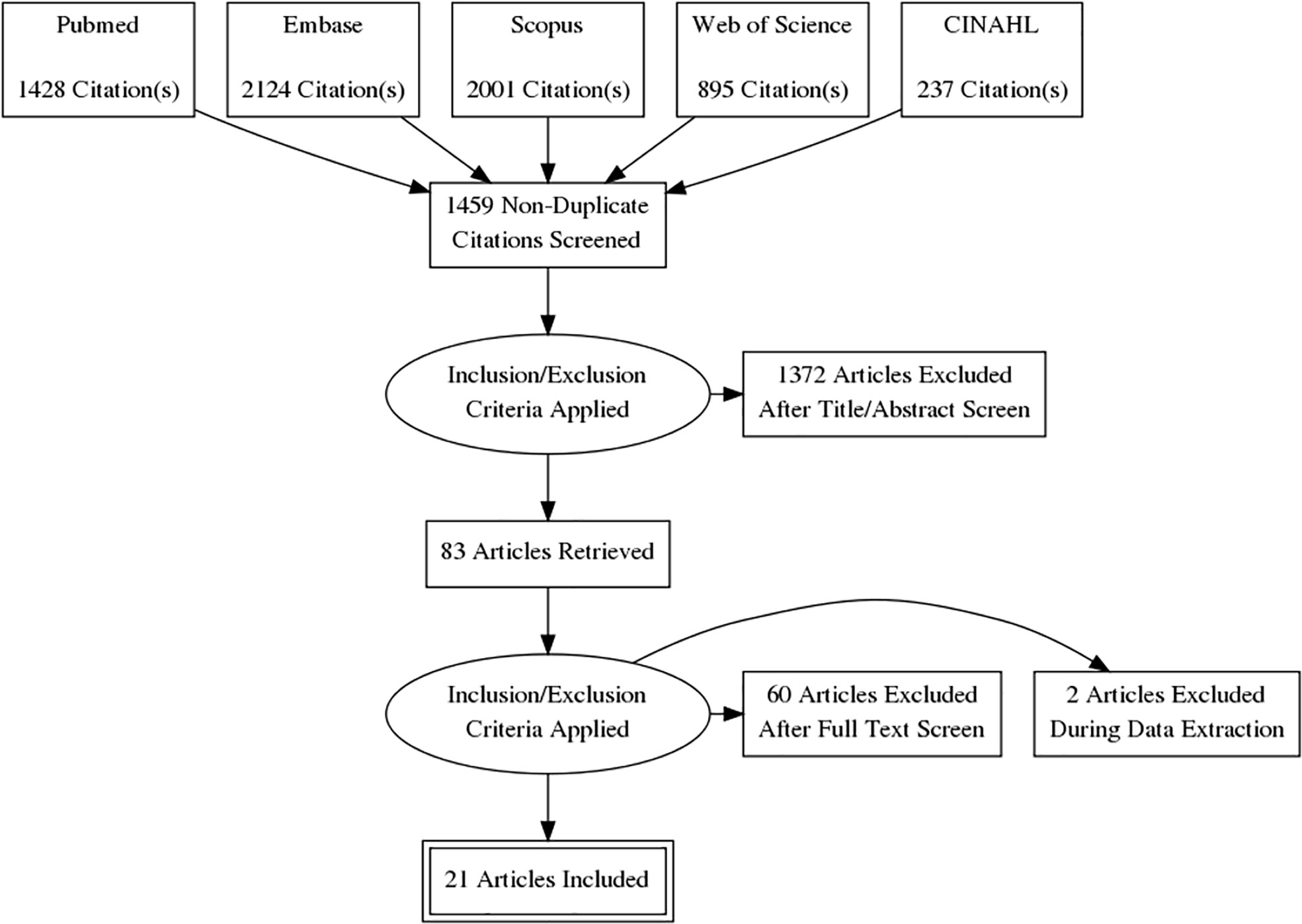
A full breakdown of the literature search appears in a PRISMA diagram (Figure 1). The initial search contained 6684 articles. 5206 duplicates were removed in EndNote. 1459 studies were screened by title and abstract, and 1372 studies were eliminated based on inclusion and exclusion criteria. Full-text review was performed for 83 articles. Sixty articles were excluded because the study did not take place in the US (n = 46), not a student population (n = 7), covered other vaccines (n = 3), did not have full text available (n = 2), duplicate (n = 1), not a health profession included in the study (n = 1), undergraduate students (n = 1), or measured the wrong outcome (n = 1). An additional 2 articles were excluded during data extraction.
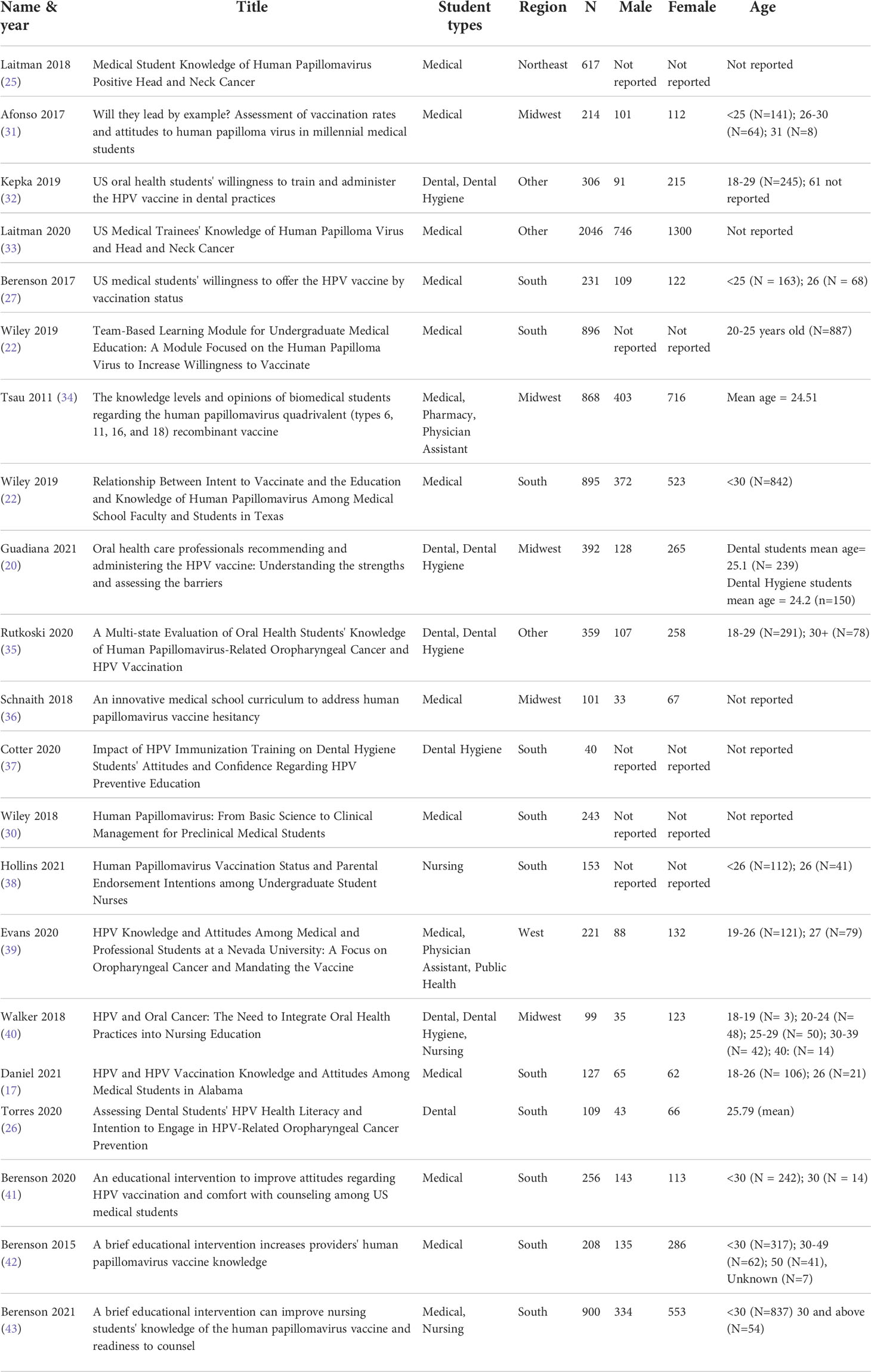
A total of 21 articles were included in the analysis (Table 3) (20, 22, 25–27, 30–43, 45, 46). Of the studies included, 20 included knowledge data, 11 included vaccine uptake, 8 included interventions, and 12 included counseling comfort. The students in the studies included medical (n=14), dental (n=7), dental hygiene (n=6), nursing (n=3), physician assistant (n=2), public health (n=1), and pharmacy (n=1). Most participants across all studies that reported gender were female (56.3%).
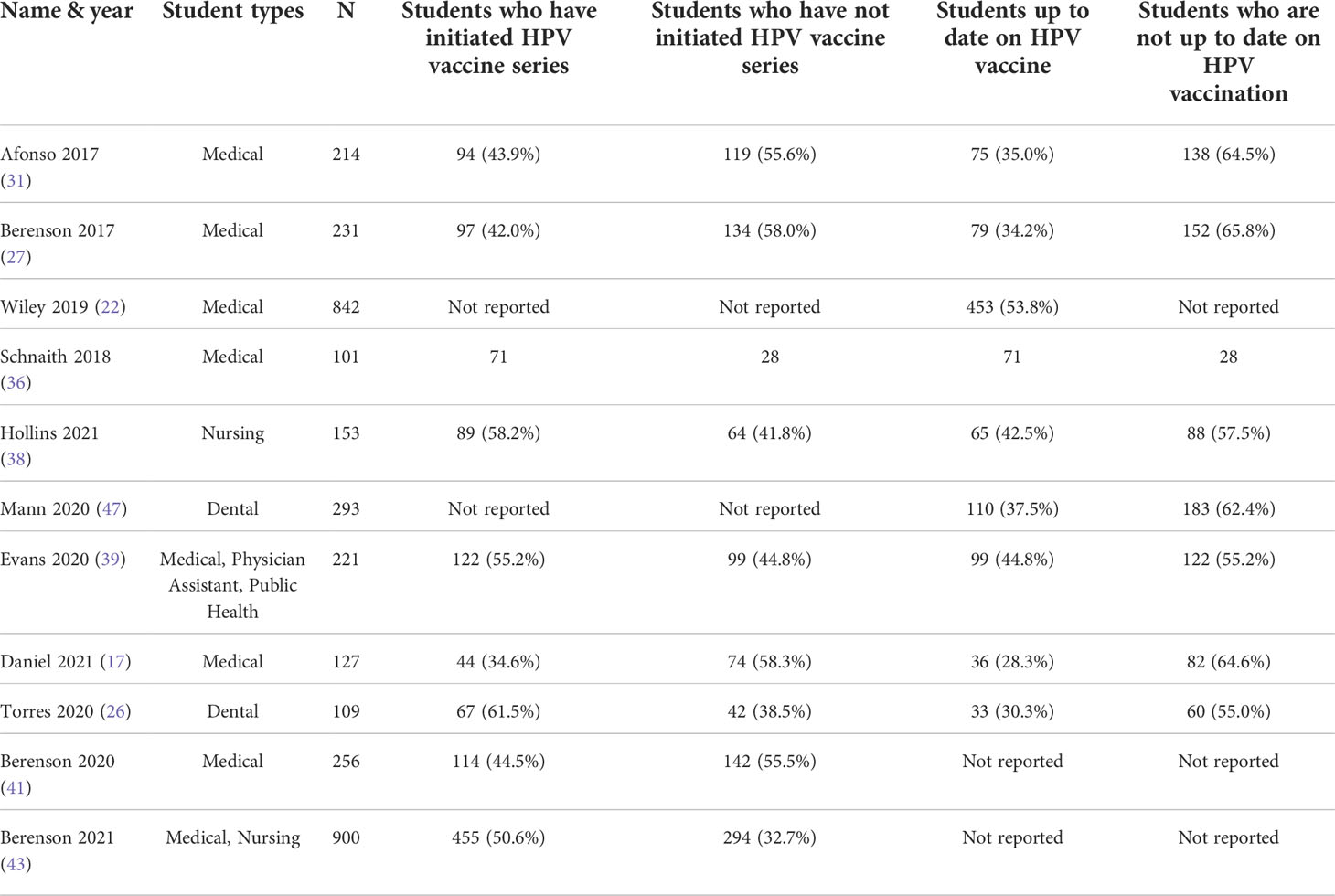
Vaccine uptake
Table 4 summarizes the vaccine uptake of participants in all studies that included this measure. Most participants were under age 30, and therefore eligible for HPV vaccination during childhood. Across studies, the rate of reported HPV vaccine series initiation ranged from 34.6% to 70.3%, and the rate of those up to date on HPV vaccination ranged from 28.3% to 58.3%. Multiple studies noted that highest rate of vaccine uptake was in participants under age 25 (27, 31, 46). In studies that reported vaccination rate by gender, female students were more likely to be vaccinated (27, 31, 46). Provider recommendation also influenced the decision to get the HPV vaccine in multiple studies (38, 47).
Knowledge
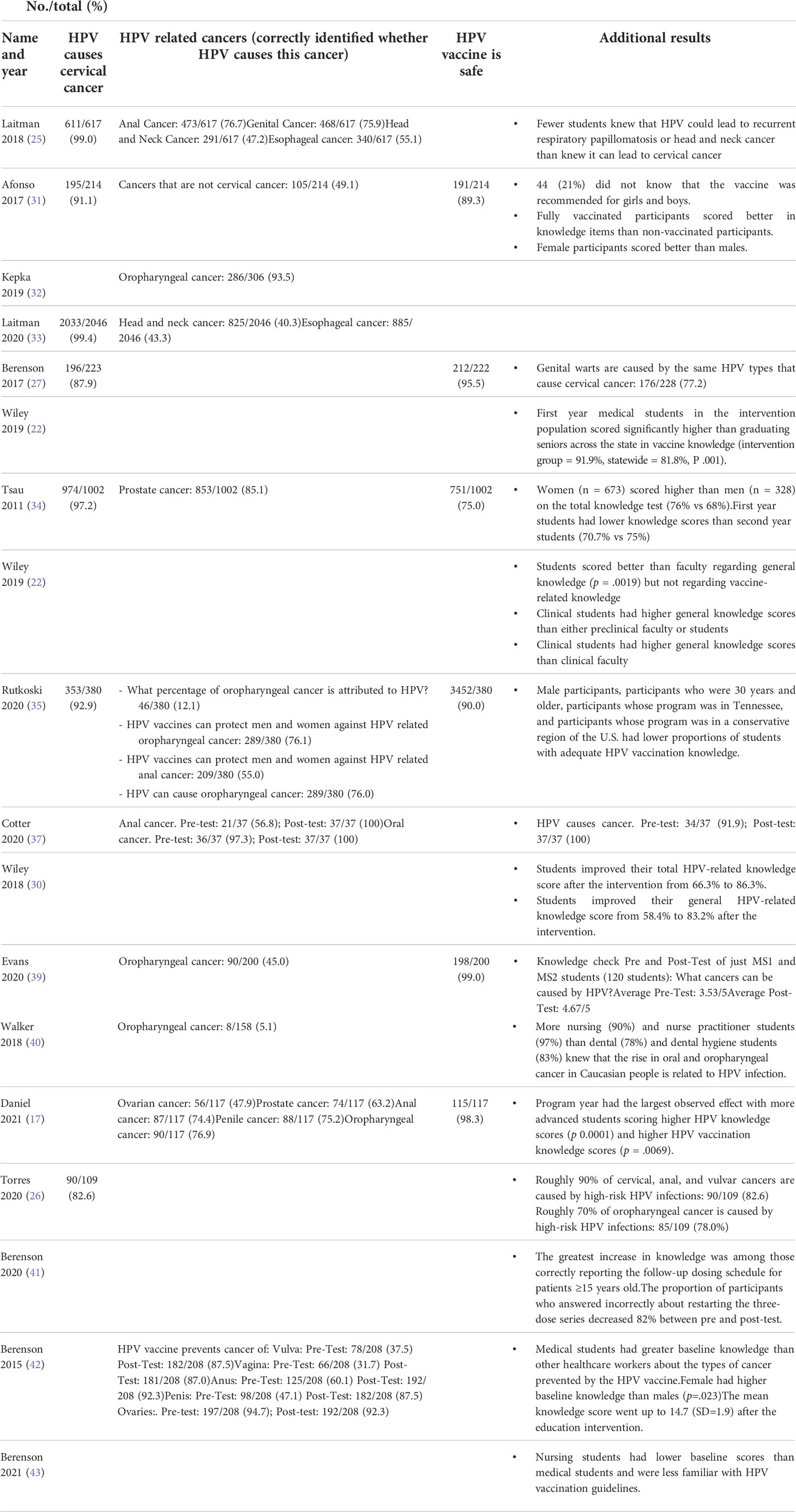
Table 5 describes the level of HPV knowledge among HPS. Knowledge gaps surrounding the link between HPV and head and neck cancers were most notable. Laitman et al. reported in two studies that 99% (611/617) and 99.4% (2033/2046) of medical students correctly identified HPV infection as a cause of cervical cancer, but only 47.2% (291/617) and 40.3% (825/2046) correctly connected HPV with head and neck cancers (25, 33). Medical, physician assistant and public health students demonstrated a similar knowledge gap regarding HPV and oropharyngeal cancers. Evans et al. found that only 45% (90/200) of medical students knew that HPV could cause oropharyngeal cancer (39). Overall, dental and dental hygiene students had greater understanding of the link between HPV and oropharyngeal cancer, ranging from 97.3% to 70% (26, 37). However, Walker et al. found that only 5.1% (8/158) of dental, dental hygiene, and nursing students knew that HPV vaccines may be effective in protecting against HPV and related oropharyngeal cancer (40).
HPS also demonstrated knowledge gaps in the vaccine dosing schedule. Berenson et al. found that only 25.1% (44/175) of medical students knew whether a patient should restart the vaccine series if their last dose was more than a year ago (27). Cotter et al. demonstrated that only 35.1% (13/37) and 37.8% (14/37) of dental hygiene students identified the correct number of doses for those under age 15 and those at or over age 15 respectively (37). Berenson et al. found that only 31.3% (80/256) of medical students knew the CDC recommended schedule of follow up doses for those 15 years or older (41).
The majority of students in each study knew that the HPV vaccine is safe, though there was a wide range between 75% (751/1002) and 99% (198/200) of HPS with this knowledge (34, 39).
Educational interventions
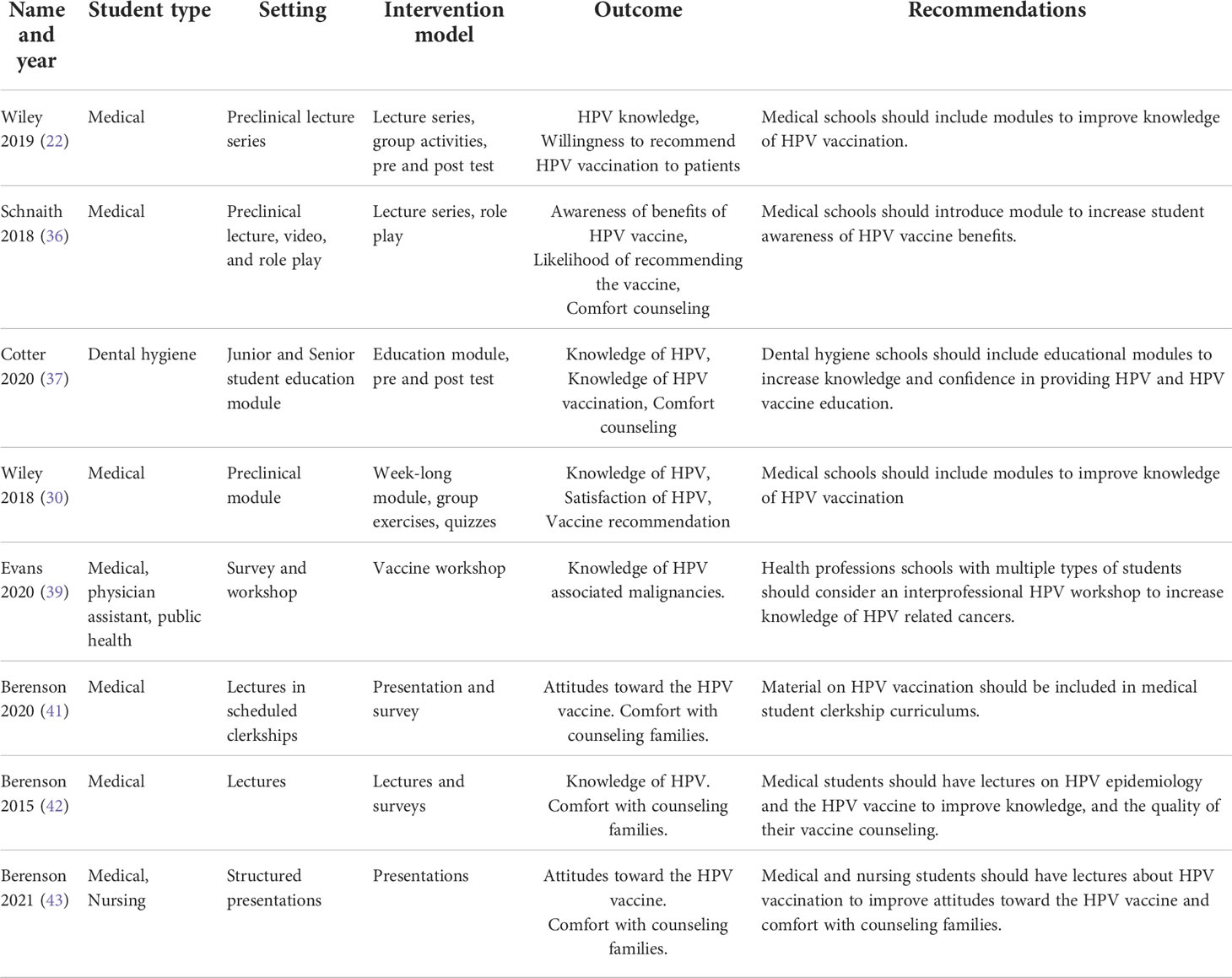
Table 6 summarizes the key findings of the studies regarding educational interventions. Most interventions combined lectures and group activities. Topics covered included HPV virology, HPV-related cancers, epidemiology, vaccines, and comfort counseling. All studies reported improved knowledge following educational interventions (36, 37, 39, 41, 42, 46).
Wiley et al. demonstrated that a team-based instructional module with video simulations and clinical vignettes improved HPV and vaccine knowledge among first year medical students (46). Students in the intervention group showed significant general knowledge improvement (from 58.4% to 85.3% P<.001) and vaccine-related knowledge (from 78.8% to 91.7% P<.001). In another study by Schnaith et al. (2018), the intervention consisted of a lecture, video and role-play simulation (36). The intervention increased awareness of the benefits of the HPV vaccine by 0.82 points on a Likert scale of 1-5.
In Berenson et al. (2015), a brief lecture presentation discussing HPV and vaccination for healthcare workers significantly improved HPV knowledge (42). Medical students participating in a 12 lecture series covering HPV and vaccination in Berenson et al., 2020 demonstrated significant improvement in knowledge and comfort counseling patients regarding HPV vaccination (41). In Berenson et al. (2021), a similar intervention was presented to nursing students covering dosing schedules, efficacy and safety of the vaccine with similar improvement in knowledge scores (43).
In Evans et al. (2020), first- and second-year medical students attended a 1.5-hour HPV vaccine workshop covering HPV and strategies to address vaccine hesitancy (39). After the workshop, students demonstrated improved scores in the area of HPV-related malignancies (mean improved from 3.53 to 4.67), transmission (3.05 to 3.87), symptoms (1.76 to 2.63), and vaccination schedule (1.21 to 1.68).
In Cotter et al. (2020), an educational intervention for dental hygiene students consisted of a one-hour educational module covering the prevalence of HPV, HPV oropharyngeal cancers, HPV vaccination and information on counseling techniques (37). Following the intervention, the mean score on the knowledge test increased from 8.75 to 13.32 (scale 0-15).
These results demonstrate that a variety of effective educational strategies for improving knowledge about HPV and HPV vaccination. While elaborate interventions such as the team-based learning modules outlined in Wiley et al. (2018) and the three-part educational curriculum created in Schnaith et al. (2019) are effective, simpler models such as the one-hour educational module discussed in Cotter et al. (2019) and the 1.5 hour workshop in Evans et al. (2020) can be effective, and may be easier for institutions to implement (31, 32, 36, 37, 39, 46–48).
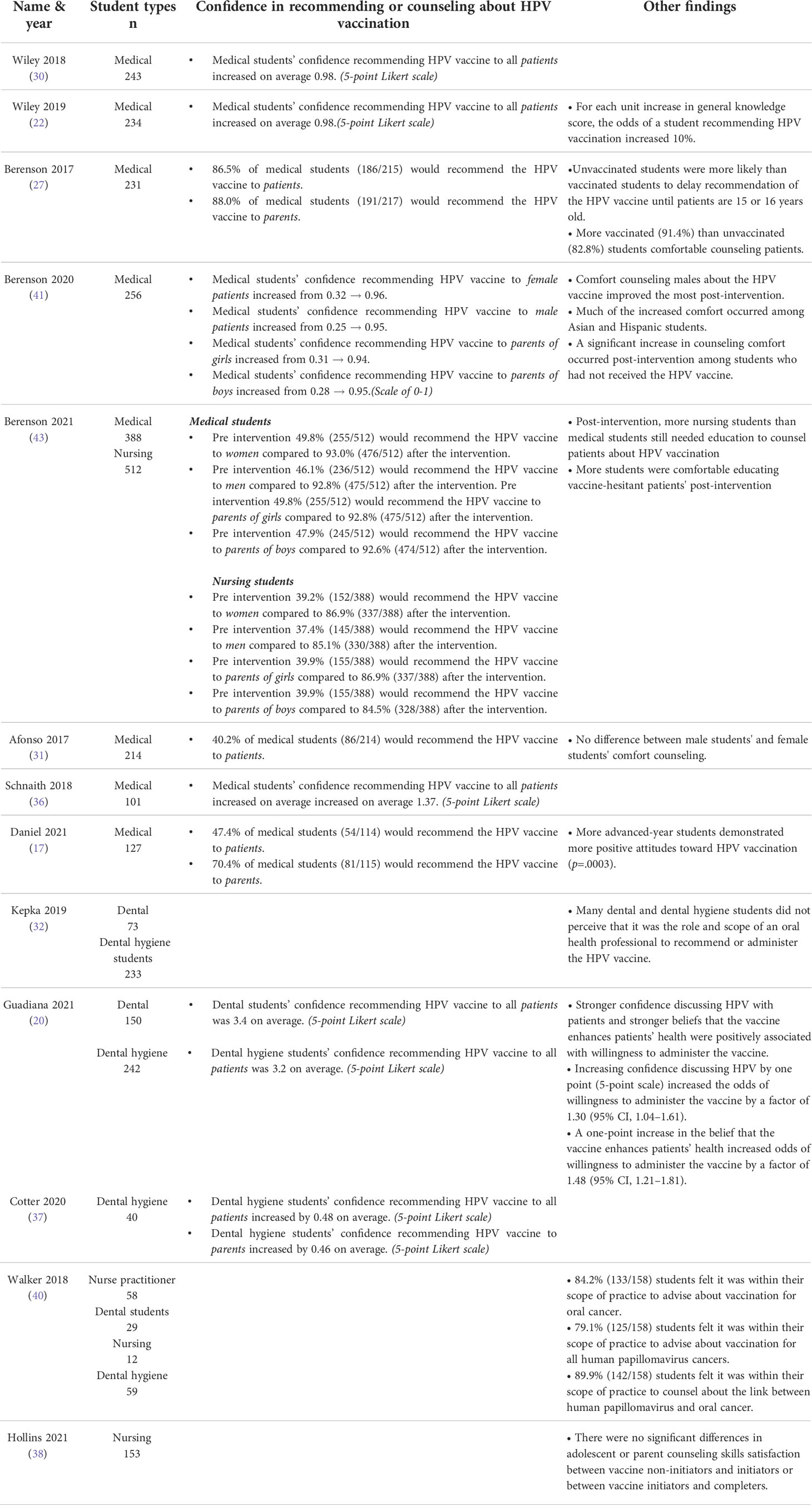
Counseling comfort
Table 7 summarizes the key findings regarding HPS comfort recommending and discussing the HPV vaccine. Among medical students, Berenson et al. found that more vaccinated (85/93 91.4%) than unvaccinated (101/122 82.8%) students agreed that they were comfortable discussing the benefits and risk of HPV vaccination (27). However, Wiley et al. found no difference in willingness to recommend the vaccine between vaccinated and unvaccinated students (46).
Wiley et al. found that medical students who were hesitant or ambivalent about recommending the HPV vaccine scored lower on the total HPV knowledge assessment (p=.026) and general HPV knowledge assessment (p=.03) compared to students who were likely to recommend vaccination (46). Similarly, Daniel et al. found that students further along in medical school demonstrated more positive attitudes toward HPV vaccination (p=.0003) (45).
Each study of medical students that included an educational intervention showed improvement in their ability to counsel others regarding HPV vaccination. Wiley et al. reported that 100% of students agreed that they would recommend the vaccine as a provider after a week-long team-based learning exercise (46). Schnaith et al. found an increase in students’ comfort conversing with HPV vaccine-hesitant parents/patients after an educational HPV curriculum (36). Berenson et al. reported significant increases in medical students’ comfort counseling parents and eligible men and women about the vaccine following HPV lectures (41). A significant increase in counseling comfort occurred among students who had not received the HPV vaccine. In another study, Berenson et al. demonstrated that medical and nursing students were significantly more comfortable educating vaccine-hesitant patients post-intervention (43). Generally, the studies found more hesitancy within vaccine counseling from non-medical HPS than medical students. Kepka et al. found that dental and dental hygiene students did not perceive that it was the role of an oral health professional to recommend or administer the HPV vaccine (32).
Studies among dental and dental hygiene students found that educational interventions improved comfort surrounding administering and discussing HPV vaccines. Guadiana et al. found that dental and dental hygiene students who were more confident in their ability to discuss HPV were more likely to be willing to administer the vaccine (OR 1.30, 95% CI 1.04–1.61) (20). Additionally, a one-point increase in the belief that the vaccine enhances patients’ health increased the students’ willingness to administer the vaccine (OR 1.48, 95% CI 1.21–1.81). Cotter et al. found that after an interactive online training module, dental hygiene students increased their confidence providing HPV vaccination counseling to patients (p =.033).
Discussion
An estimated 79 million people in the United States are infected with HPV, and in individuals not able to clear the virus, leads to cancer. Despite significant data demonstrating HPV vaccination efficacy, vaccination rates remain stagnant; and HPV related oropharyngeal and anal/rectal cancers are on the rise, particularly among men (49). Our study systematically examines HPV vaccine uptake, knowledge, counseling comfort and interventions to increase HPV knowledge among HPS, the next generation of healthcare providers.
The rates of HPV vaccine series initiation across studies ranged from 34.6% to 70.3%, and the rate of those up to date on HPV vaccination ranged from 28.3% to 58.3% (27, 31, 46). Rates of vaccination were the highest among those under 25, and female (27, 31, 46). Moreover, provider recommendation of the vaccine influenced the decision to get vaccinated in multiple studies – emphasizing why educating students as the next generation of providers is so critical (38, 47). In order to achieve the goals of Healthy People 2030 and the World Health Organization (WHO) goal to eradicate cervical cancer by 2030, increasing the vaccination rate to 90% is essential (48). A strong healthcare workforce of HPV vaccine advocates is critical to this mission.
While students consistently displayed awareness that HPV causes cervical cancer (99%), many lacked knowledge of the ability of HPV to cause other cancers including head and neck cancer (40-47%) and oropharyngeal cancer (45%) (33, 40). Most students did know that HPV vaccination is safe (75-99%) (34, 39). Other knowledge gaps about HPV vaccination included dosing schedules, age ranges, boys needing vaccination, and whether to initiate the vaccine series prior to sexual activity. However, while rates of cervical cancer have decreased from improved screening and HPV vaccination, the US still lags behind other developed nations in their progress towards cervical cancer eradication (50).
Educational interventions varied in format but were consistently effective in increasing knowledge of HPV. One team-based instruction module significantly increased general HPV knowledge, HPV vaccine related knowledge, and likelihood of vaccine recommendation (46). A different workshop, which also covered vaccine hesitancy, significantly improved knowledge of HPV related cancers, symptoms, and vaccine dosing schedules (37). While many of the interventions were time intensive, the shorter interventions also increased knowledge. Finding a balance between length of intervention necessary to provide sufficient education but remain feasible to implement amongst the many topics covered in a medical education is essential.
Additionally, comfort counseling patients about HPV vaccination was low – but increased following specific interventions targeting this objective. Students across studies cited similar barriers to HPV vaccine uptake to their patients including parental decline of the vaccine, not being recommended the vaccine by a healthcare provider (27, 38, 45). Moreover, previous studies have shown that students who were vaccinated against HPV were more likely to recommend vaccination, especially to adolescents (27). Following educational interventions, more students felt comfortable recommending HPV vaccination. It is critical to target efforts to increase vaccination rates amongst students in the health professions. This should include availability of the HPV vaccine at school sponsored health services and ensuring that providers at these sites are educated about the importance of HPV vaccination. Additionally, since most health professional schools require flu vaccination for students each year, schools should consider offering HPV vaccination alongside flu vaccinations. HPV vaccination prevents not only HPV related cancers but also pre-invasive disease such as cervical dysplasia, which in women of reproductive age, can be quite devastating.
Limitations of this analysis include that most are single institutional studies and are thus subject to any bias resulting from the studies themselves. The risk of bias has been minimized through screening prior to inclusion. Additionally, it is of note that there are multiple studies from the same authors because there are investigators who have conducted multiple studies in this area.
Future studies should focus on ways to target vaccine uptake in HPS and expand upon existing knowledge interventions to implement better education on a broader scale. This education should utilize an interprofessional approach is vital to expanding the number of knowledgeable professionals counseling and offering HPV vaccination to prevent HPV-related cancers. The papers reviewed in this analysis demonstrated that various educational modalities of different lengths effectively increase knowledge of HPV and HPV vaccination. Further studies should focus on educational methods to help determine optimal approaches by objective measures such as a significant increase in HPV vaccination. Ultimately, we must take active efforts to improve the quality of education provided. Taking these steps to enhance HPS education is critical to lowering the number of missed opportunities for HPV vaccination in a variety of healthcare settings.
Conclusion
Across HPS, major gaps persist in HPV vaccine uptake, knowledge, and counseling comfort. It is critical to target vaccine uptake in this population, including ensuring availability of vaccination for students. Educational institutions must make education about the HPV vaccine a priority in both preclinical and clinical curriculums. This study highlights the need for interventions to improve HPV vaccination uptake and education on HPV in HPS to train healthcare professionals that strongly recommend HPV vaccination to prevent cancer.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
ML and MH had full access to all the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design, all authors. Acquisition, analysis, or interpretation of data, all authors. Drafting of the manuscript, ML, LF, and KL. Critical revision of the manuscript for important intellectual content, all authors. Statistical analysis, ML, LF, and KL. Administrative, technical, or material support, MH and PJ. Supervision, MH and PJ. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors thank Dr. Barbara Sorondo and John Reynolds from Calder Library for consultation on study methodology.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. CDC. Cancers associated with human papillomavirus, united States—2014–2018 (2021). Available at: https://www.cdc.gov/cancer/uscs/about/data-briefs/no26-hpv-assoc-cancers-UnitedStates-2014-2018.htm (Accessed January 29, 2022).
2. International Agency for Research On Cancer. Cancers attributable to infections . International Agency for Research on Cancer. Available at: https://gco.iarc.fr/causes/infections/tools-pie?mode=2&sex=0&population=who&continent=0&country=0&population_group=0&cancer=0&key=attr_cases&lock_scale=0&pie_mode=1&nb_results=5 (Accessed January 29, 2022).
3. CDC. Cancers associated with human papillomavirus, united States—2012–2016 (2012). Available at: https://www.cdc.gov/cancer/hpv/ (Accessed December 26, 2021).
4. Liao C-I, Caesar MAP, Chan C, Richardson M, Kapp DS, Francoeur AA, et al. HPV associated cancers in the united states over the last 15 years: Has screening or vaccination made any difference? J Clin Oncol (2021) 39(15_suppl):107–7. doi: 10.1200/jco.2021.39.15_suppl.107
5. Miller NB, Roberts J. Clinical review of biologics license application for human papillomavirus 16, 18 L1 virus like particle vaccine, AS04 adjuvant-adsorbed (Cervarix) (2006).
6. Lei J, Ploner A, Elfström KM, Wang J, Roth A, Fang F, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med (2020) 383(14):1340–8. doi: 10.1056/nejmoa1917338
7. Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: Updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep (2019) 68(32):698–702. doi: 10.15585/mmwr.mm6832a3
8. Attia AC, Wolf J, Núñez AE. On surmounting the barriers to HPV vaccination: we can do better. Ann Med (2018) 50(3):209–25. doi: 10.1080/07853890.2018.1426875
9. Pingali C, Yankey D, Elam-Evans LD, Markowitz LE, Williams CL, Fredua B, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years — united states, 2020. MMWR Recomm Rep (2021) 70(35):1184–90. doi: 10.15585/mmwr.mm7035a1
10. Sonawane K, Lin YY, Damgacioglu H, Zhu Y, Fernandez ME, Montealegre JR, et al. Trends in human papillomavirus vaccine safety concerns and adverse event reporting in the united states. JAMA Netw Open (2021) 4(9):e2124502–e2124502. doi: 10.1001/jamanetworkopen.2021.24502
11. Bednarczyk RA. Addressing HPV vaccine myths: practical information for healthcare providers. Hum Vaccines Immunother (2019) 15(7-8):1628–38. doi: 10.1080/21645515.2019.1565267
12. Kearney MD, Selvan P, Hauer MK, Leader AE, Massey PM. Characterizing HPV vaccine sentiments and content on instagram. Heal Educ Behav (2019) 46(2_suppl):37–48. doi: 10.1177/1090198119859412
13. Massey PM, Kearney MD, Hauer MK, Selvan P, Koku E, Leader AE. Dimensions of misinformation about the HPV vaccine on instagram: Content and network analysis of social media characteristics. J Med Internet Res (2020) 22(12):e21451. doi: 10.2196/21451
14. Hughes CT, Kirtz S, Ramondetta LM, Lu Q, Cho D, Katzin C, et al. Designing and implementing an educational social media campaign to increase HPV vaccine awareness among men on a Large college campus. Am J Heal Educ (2020) 51(2):87–97. doi: 10.1080/19325037.2020.1722297
15. Kessels SJM, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: A systematic review. Vaccine (2012) 30(24):3546–56. doi: 10.1016/j.vaccine.2012.03.063
16. Whelan NW, Steenbeek A, Martin-Misener R, Scott J, Smith B, D’Angelo-Scott H. Engaging parents and schools improves uptake of the human papillomavirus (HPV) vaccine: Examining the role of the public health nurse. Vaccine (2014) 32(36):4665–71. doi: 10.1016/j.vaccine.2014.06.026
17. Daniel CL, Lawson F, Vickers M, Green C, Wright A, Coyne-Beasley T, et al. Enrolling a rural community pharmacy as a vaccines for children provider to increase HPV vaccination: a feasibility study. BMC Public Health (2021) 21(1):1–10. doi: 10.1186/s12889-021-11304-8
18. Cebollero J, Walton SM, Cavendish L, Quairoli K, Cwiak C, Kottke MJ. Evaluation of human papillomavirus vaccination after pharmacist-led intervention: A pilot project in an ambulatory clinic at a Large academic urban medical center. Public Health Rep (2020) 135(3):313–21. doi: 10.1177/0033354920914340
19. Fava JP, Colleran J, Bignasci F, Cha R, Kilgore PE. Adolescent human papillomavirus vaccination in the united states: Opportunities for integrating pharmacies into the immunization neighborhood. Hum Vaccines Immunother (2017) 13(8):1844–55. doi: 10.1080/21645515.2017.1325980
20. Guadiana D, Kavanagh NM, Squarize CH. Oral health care professionals recommending and administering the HPV vaccine: Understanding the strengths and assessing the barriers. PloS One (2021) 16(3):e0248047. doi: 10.1371/journal.pone.0248047
21. Nelson JD, Lubker I, Bowers L, Neville B. Elevating dental training to prioritize prevention efforts for reducing HPV-related oropharyngeal cancer incidence. J Dent Educ (2021) 85(6):835–46. doi: 10.1002/jdd.12577
22. Wiley R, Shelal Z, Urbauer D, Bernard C, Ramondetta L. Relationship between intent to vaccinate and the education and knowledge of human papillomavirus among medical school faculty and students in Texas. Tex Med (2019) 115(1):e1.
23. Hurley LP, O’Leary ST, Markowitz LE, Crane LA, Cataldi JR, Brtnikova M, et al. US Primary care physicians’ viewpoints on HPV vaccination for adults 27 to 45 years. J Am Board Fam Med (2021) 34(1):162–70. doi: 10.3122/jabfm.2021.01.200408
24. Leung SOA, Akinwunmi B, Elias KM, Feldman S. Educating healthcare providers to increase human papillomavirus (HPV) vaccination rates: A qualitative systematic review. Vaccine X. (2019) 3:100037. doi: 10.1016/j.jvacx.2019.100037
25. Laitman BM, Oliver K, Genden E. Medical student knowledge of human papillomavirus-positive head and neck cancer. JAMA Otolaryngol - Head Neck Surg (2018) 144(4):380–2. doi: 10.1001/jamaoto.2017.3089
26. Torres E, Richman A, Wright W, Wu Q. Assessing dental students’ HPV health literacy and intention to engage in HPV-related oropharyngeal cancer prevention. J Cancer Educ (2020). doi: 10.1007/s13187-020-01905-z
27. Berenson AB, Hirth JM, Fuchs EL. US Medical student’s willingness to offer the HPV vaccinne by vaccination status. Vaccine (2017) 35(9):1212–5. doi: 10.1016/j.vaccine.2017.01.028.US
28. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst Rev (2021) 10(89):1–11. doi: 10.1186/s13643-021-01626-4
29. Aromataris E, Munn Z, Moola S, et al. Checklist for analytical cross sectional studies (2020). Available at: https://jbi.global/critical-appraisal-tools (Accessed July 22, 2021).
30. Wiley R, Shelal Z, Bernard C, Urbauer D, Toy E, Ramondetta L. Human papillomavirus: From basic science to clinical management for preclinical medical students. MedEdPORTAL J Teach Learn Resour (2018) 14:10787. doi: 10.15766/mep_2374-8265.10787
31. Afonso NM, Kavanagh MJ, Swanberg SM, Schulte JM, Wunderlich T, Lucia VC. Will they lead by example? assessment of vaccination rates and attitudes to human papilloma virus in millennial medical students. BMC Public Health (2017) 17(1):35. doi: 10.1186/s12889-016-3969-x
32. Kepka D, Rutkoski H, Pappas L, Tay DL, Winkler JR, Dixon B, et al. US Oral health students’ willingness to train and administer the HPV vaccine in dental practices. Prev Med Rep (2019) 15:100957. doi: 10.1016/j.pmedr.2019.100957
33. Laitman BM, Ronner L, Oliver K, Genden E. US Medical trainees’ knowledge of human papilloma virus and head and neck cancer. Otolaryngol - Head Neck Surg (United States) (2020) 162(1):56–9. doi: 10.1177/0194599819886117
34. Tsau K, Reutzel TJ, Wang S, Qui�ones A, Nguyen P, Hasan S, et al. The knowledge levels and opinions of biomedical students regarding the human papillomavirus quadrivalent (types 6, 11, 16, and 18) recombinant vaccine. J Pharm Pract (2011) 24(2):223–34. doi: 10.1177/0897190010387933
35. Rutkoski H, Tay DL, Dixon BL, Pinzon LM, Mooney R, Winkler JR, et al. A multi-state evaluation of oral health students’ knowledge of human papillomavirus-related oropharyngeal cancer and HPV vaccination. J Cancer Educ (2020) 35(5):1017–25. doi: 10.1007/s13187-019-01561-y
36. Schnaith AM, Evans EM, Vogt C, Tinsay AM, Schmidt TE, Tessier KM, et al. An innovative medical school curriculum to address human papillomavirus vaccine hesitancy. Vaccine (2018) 36(26):3830–5. doi: 10.1016/j.vaccine.2018.05.014
37. Cotter JC, Wilson KJ, Mallonee LF. Impact of HPV immunization training on dental hygiene students’ attitudes and confidence regarding HPV preventive education. J Dent Educ (2020) 84(1):88–93. doi: 10.21815/jde.019.164
38. Hollins A, Wardell D, Fernandez ME, Markham C, Guilamo-Ramos V, Maria DS. Human papillomavirus vaccination status and parental endorsement intentions among undergraduate student nurses. Int J Environ Res Public Health (2021) 18(6):1–10. doi: 10.3390/ijerph18063232
39. Evans L, Matley E, Oberbillig M, Margetts E, Darrow L. HPV knowledge and attitudes among medical and professional students at a Nevada university: A focus on oropharyngeal cancer and mandating the vaccine. J Cancer Educ (2020) 35(4):774–81. doi: 10.1007/s13187-019-01529-y
40. Walker KK, Jackson RD, Edwards PC, Vadaparampil ST. HPV and oral cancer: The need to integrate oral health practices into nursing educatiion. Clin J Oncol Nurs. (2018) 22(6):E166–173. doi: 10.1097/00125480-199709000-00024
41. Berenson AB, Hirth JM, Fuchs EL, Chang M, Rupp RE. An educational intervention to improve attitudes regarding HPV vaccination and comfort with counseling among US medical students. Hum Vaccin Immunother (2020) 16(5):1139–44. doi: 10.1080/21645515.2019.1692558
42. Berenson AB, Rahman M, Hirth JM, Rupp RE, Sarpong KO. A brief educational intervention increases providers’ human papillomavirus vaccine knowledge. Hum Vaccines Immunother (2015) 11(6):1331–6. doi: 10.1080/21645515.2015.1022691
43. Berenson AB, Hirth JM, Chang M, Kuo YF, Richard P, Jones DL. A brief educational intervention can improve nursing students’ knowledge of the human papillomavirus vaccine and readiness to counsel. Hum Vaccines Immunother (2021) 17(7):1952–60. doi: 10.1080/21645515.2020.1852871
44. Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. Gesundheitswesen (2016) 78(3):175–88. doi: 10.1055/s-0041-111066
45. Daniel CL, McLendon L, Green CL, Anderson KJ, Pierce JY, Perkins A, et al. HPV and HPV vaccination knowledge and attitudes among medical students in Alabama. J Cancer Educ (2021) 36(1):168–77. doi: 10.1007/s13187-019-01613-3
46. Wiley R, Shelal Z, Bernard C, Urbauer D, Toy E, Ramondetta L. Team-based learning module for undergraduate medical education: a module focused on the human papilloma virus to increase willingness to vaccinate. J Cancer Educ (2019) 34(2):357–62. doi: 10.1007/s13187-017-1311-7
47. Mann SK, Kingsley K. Human papillomavirus (HPV) vaccine knowledge, awareness and acceptance among dental students and post-graduate dental residents. Dent J (2020) 8(2):1–10. doi: 10.3390/dj8020045
48. Healthy People 2030. Increase the proportion of adolescents who get recommended doses of the HPV vaccine — IID−08 (2021). Available at: https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-adolescents-who-get-recommended-doses-hpv-vaccine-iid-08 (Accessed March 1, 2022).
49. Liao CI, Francoeur AA, Kapp DS, Caesar MAP, Huh WK, Chan JK. Trends in human papillomavirus–associated cancers, demographic characteristics, and vaccinations in the US, 2001-2017. JAMA Netw Open (2022) 5(3):e222530–e222530. doi: 10.1001/JAMANETWORKOPEN.2022.2530
Keywords: HPV vaccination, cancer prevention, cervical cancer, medical education, interprofesssional education, vaccine hesistancy, public health
Citation: Levy MS, Finch L, Lindsay KA, Jeudin P and Huang M (2022) Leveraging teachable moments in cancer prevention by improving HPV vaccination in health professional students (HPS): A systematic review. Front. Oncol. 12:978843. doi: 10.3389/fonc.2022.978843
Received: 26 June 2022; Accepted: 01 August 2022;
Published: 29 August 2022.
Edited by:
Sarah M. Temkin, National Institutes of Health (NIH), United StatesReviewed by:
Zohre Momenimovahed, Qom University of Medical Sciences, IranNicholas Harris Schluterman, University of Maryland, United States
Copyright © 2022 Levy, Finch, Lindsay, Jeudin and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marilyn Huang, m.huang@med.miami.edu
 Morgan S. Levy
Morgan S. Levy Lindsey Finch
Lindsey Finch Kara A. Lindsay1
Kara A. Lindsay1 Marilyn Huang
Marilyn Huang